Duty of care vs dignity of risk
After a traumatic brain injury, life takes a significant turn for our clients. For some, the change to their cognitive skills means they are no longer able to make independent decisions. For others, it means they may need help to consider all their options before making decisions.
It is a really big issue, for both the person and individuals/organisations now part of the person’s world, helping them to make life decisions. Before getting in a complete flap, there are legal responsibilities and definitions we, as health care workers, are obliged to meet. So let’s start there; by defining these two big, really important concepts:
Duty of care:
This is a legal term, with clearly defined meaning. Duty of care is the responsibility of organisations (and the people who work in them) to ensure they do no harm to the people they support. But it doesn’t mean the organisation has to protect the person from themselves.
Dignity of risk:
Dignity of risk refers to the right of an individual to make choices and take risks in order to learn, grow and have better quality of life.
Inherent to the idea of dignity of risk is the idea that life experiences come with an element of risk, which even the best planning and support cannot eliminate.
The right to make choices for self-determination is assumed until it is established that assistance is required.
A delicate balance
The intersection of duty of care and dignity of risk for people in need of support is a very grey area indeed. There are further legal parameters to help define the edges. It is not the role of the health or support team to decide who has capacity to make financial, health, or life decisions. For our clients, this is often a formal process, where the Guardianship Tribunal outlines the specific areas in which the person has capacity to make decisions and what they don’t. This process also identifies the person(s) who are allowed to make decisions on a person’s behalf. The tricky bit comes after this decision has been made. This is because allied health practitioners and support people play a significant role in assisting the person with impaired capacity for decision-making, to make assisted decisions.
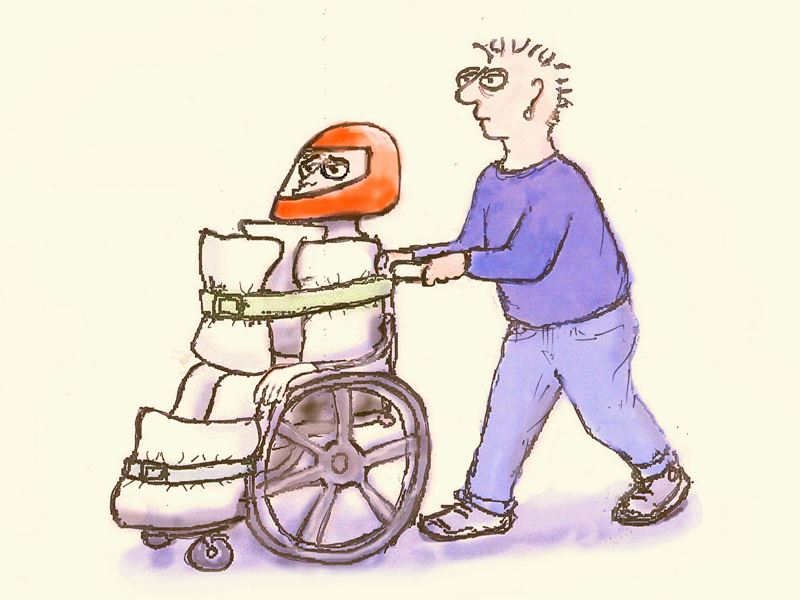
I think another key issue happens at this point. As a generalisation, before sustaining a brain injury, many of our clients are by nature, risk-takers. Conversely, many of the people providing services and support after the accident are risk-averse in nature. This difference in natural inclinations can cause huge disparity between the level of risk individuals are comfortable with allowing on behalf of the person they support.
At this point, it is useful to go back to the guidelines from the Public Guardian about assessing capacity for decision making, and remind ourselves that:
- Capacity is decision specific
- It is important to assess the person’s capacity to make the decision, NOT the decision they are making.
I don’t usually include references from literature in these posts, but this one was so nice I couldn’t help myself…Anthony (2000)[1] states: “the notion that one has options from which to choose is often more important than the particular option one initially selects.”
Perhaps one of the questions we need to ask ourselves is, “What level of risk would this person have been comfortable with before they needed help to make decisions?” If that choice doesn’t put them at risk of serious injury, it might be the right decision for them. After all, as rehab providers, our job is to help the individual be as close to their pre-injury self as possible.
Maybe that grey area of duty of care versus dignity of risk has a silver lining after all.
 Rehab Connection
Rehab Connection 